
Addison’s disease in dogs is an endocrine disease (hormonal). It’s rarely seen in humans and very rarely seen in cats.
Sometimes called “the Great Pretender,” Addison’s disease generally affects middle-aged, female dogs, and there is definitely a breed predilection — the Standard Poodle being overrepresented.
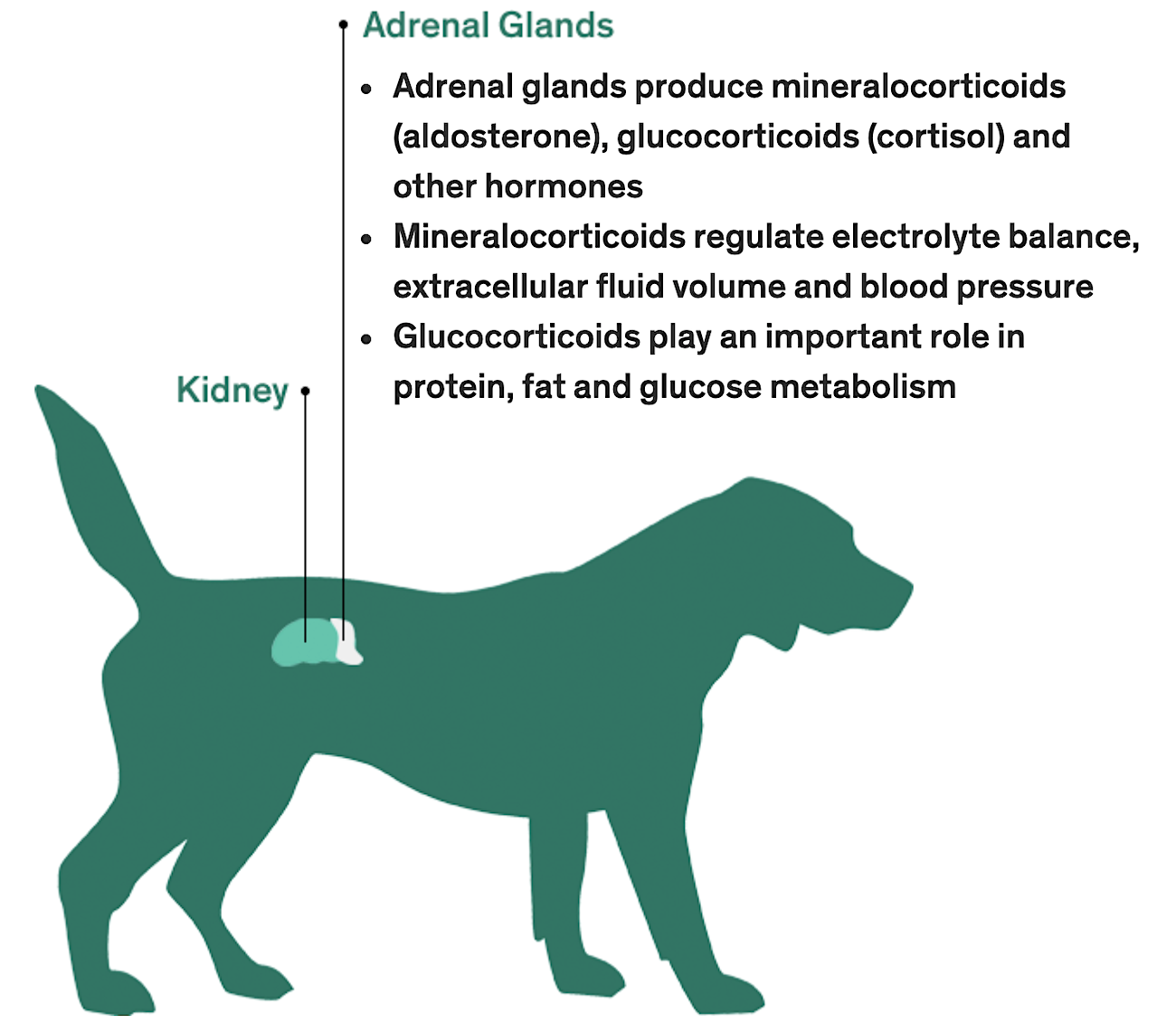
Addison’s disease is also called hypoadrenocorticism. When a dog is affected, the adrenal glands (adrenocortex) underfunction (hypo).
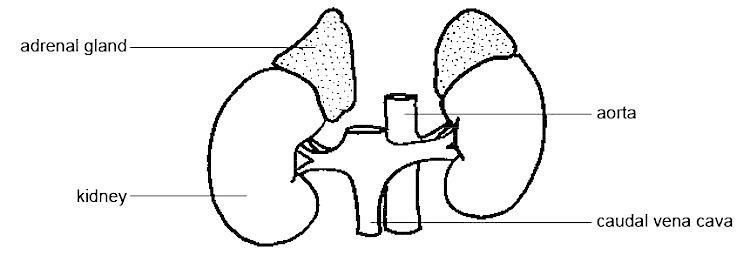
Dogs have 2 adrenal glands near each kidney. These glands secrete a few hormones that are necessary to sustain life: mineralocorticoids, glucocorticoids and androgens.
OK, so what does that mean?
Basically, the true story of how the adrenals function and all the hormonal pathways associated with hormonal diseases like Addison’s disease in dogs is, well, complicated.
So, my goal in this article? To simplify it for you.
Keep reading to discover lots of helpful information about Addison’s disease in dogs …
Addison’s Disease in Dogs: Some Basic Facts
- It can be either primary or secondary. Primary is the most common form.
- It can be typical or atypical, and typical is the most common form.
- Addison’s disease develops occasionally in dogs being treated for Cushing’s disease. If a Cushing’s dog receives too much medication — Vetoryl (trilostane) or Lysodren (mitotane) — the result can be Addison’s.
- Symptoms do not manifest until almost 90% of the adrenal glands are destroyed.
- A small percentage of dogs suffer an Addisonian crisis, which is a true medical emergency. These patients are severely dehydrated and can be almost comatose.
- Once diagnosed correctly, Addison’s disease can be treated and most dogs will live a normal, happy and healthy life as long as they get the proper dose of medication.

Symptoms of Addison’s Disease in Dogs
Symptoms include:
- Lethargy
- Weakness
- Anorexia
- Vomiting and/or diarrhea
- Gradual weight loss
- Thirst
- Shaking
- Depression
These symptoms are vague in most dogs, and the disease has a gradual onset. Addison’s is called “the Great Pretender” because it mimics many other conditions.
To complicate matters more, the above symptoms can wax and wane:
- People may not get too worried, for example, if their dog shows some fatigue on Tuesday but then bounces back on Wednesday. Or maybe there was some vomiting last week but then it resolved.
- Likewise, a veterinarian may not be thinking Addison’s, a fairly uncommon disease, when a client says, “Well, my dog seems a little tired sometimes but then it goes away.” Or, “My dog vomited a couple times in the past month but then ate normally.”
We vets hear these complaints all the time, all day long. Clearly, a vet may not recommend a full workup if the complaint seems mild. Or the client might decline blood work if their dog doesn’t seem really ill.
So, why would the symptoms wax and wane?
It comes down to stress.
Stress plays a big part in the life of a dog with Addison’s disease because their body cannot deal well with stress. A stressful situation can make the symptoms more noticeable.
Stress can mean anything from the dog having to deal with hot weather; exertion such as a longer walk or excessive play during exercise; or emotional stress such as a thunderstorm, changes in the daily routine or families going away.
Addisonian Crisis
Occasionally, a dog can become acutely ill from Addison’s disease, and this is a true emergency.
Was YOUR Pet Food Recalled?
Check Now: Blue Buffalo • Science Diet • Purina • Wellness • 4health • Canine Carry Outs • Friskies • Taste of the Wild • See 200+ more brands…

If the adrenals suddenly fail to produce almost any hormones at all, a dog will be in an emergency state — a crisis.
Symptoms of Addisonian crisis include:
- Inability to stand
- Mental depression to almost comatose
- Severe, life-threatening dehydration
- Cardiac abnormalities due to severe electrolyte abnormalities
- Shock
A dog in an Addisonian crisis must get to a veterinary hospital immediately, preferably a hospital with a critical care unit. Addison’s disease will probably be diagnosed quickly.
Treatment includes intravenous fluids, supplementation with glucocorticoids, and close monitoring of blood pressure and any cardiac abnormalities.
With intensive care, these dogs are usually saved.

Diagnosis of Addison’s Disease in Dogs
Initial blood work (a chemistry profile and a complete blood count) will often give big clues that the dog may be an Addisonian.
- Electrolytes are abnormal in about two-thirds of affected dogs, specifically high potassium and low sodium. (High potassium is what can cause cardiac abnormalities.)
- Kidney function is abnormal in 95% of dogs, possibly leading to a misdiagnosis of kidney disease rather than Addison’s. Once the Addison’s is treated, the kidney function should return to normal.
- An ACTH stimulation test, something that can be completed in about 1 hour, confirms whether or not the dog has Addison’s disease.
- There may also be a slow heart rate and/or weak pulses.
- If radiographs are taken, the heart may often look small due to severe dehydration.
- An EKG may be abnormal.
How We Treat It
The most important thing you need to understand is that treatment for Addison’s disease in dogs is lifelong. The disease is not curable, but it is highly manageable.
Treatment consists of replacing the hormonal substances that the body is not making for itself:
- Glucocorticoids must be replaced with a drug called prednisone. These are also called corticosteroids. Once regulated, many dogs don’t need to continue on prednisone or they take it only in times of stress.
- Mineralocorticoids must be replaced, and this can be given in daily pill form or by injection every 3–4 weeks. Most dogs do very well on the injection. Dogs must be supplemented with mineralocorticoids for the rest of their lives.

But Doesn’t Prednisone Have Side Effects?
Many people hear “prednisone” and think of side effects and all the warnings they have heard associated with this drug.
This is not a worry when giving prednisone to a dog with Addison’s disease.
When using prednisone in a non-Addisonian to treat allergies, autoimmune disease, cancer, skin disease, etc., you are giving the dog additional prednisone to treat disease. These dogs have a normal amount of glucocorticoids but are being given additional prednisone — which can have side effects.
Giving prednisone to a dog with Addison’s disaese, however, is very different because you are supplying what the body cannot make itself.
Generally, dogs need to take only a very small amount of prednisone to feel good. If side effects from prednisone do occur, the dose can be lowered further or given every other day, or another steroid can be tried.
Managing Stress in Dogs With Addison’s Disease
Stressful situations can send a stable Addisonian into a crisis.
Stress could be caused by:
- Boarding
- Holidays
- Travel
- Fireworks or thunderstorms
- Veterinary visits or procedures
- Loss of a caregiver
Vets recommend giving prednisone during these times to Addisonian dogs who are not regularly receiving it, as well as increasing the prednisone dose in dogs who take a small amount daily.
In a normal dog, stress induces the body to release excessive glucocorticoids to deal with the stressful situation.
For an Addisonian who becomes stressed, though, the body cannot produce those glucocorticoids to help deal with the stress. These dogs may go into crisis in times of stress if not given prednisone.

Which Dog Breeds Are Most Likely to Get Addison’s Disease?
Although any dog can develop Addison’s disease, around 70% of affected dogs are female. About 80% are younger than 7 years old.
Breeds with an increased risk of Addison’s disease include:
- Standard Poodle
- Soft-Coated Wheaten Terrier
- West Highland White Terrier
- Rottweiler
- Great Dane
- Bearded Collie
- Portuguese Water Dog
- Labrador Retriever
- Leonberger
- Great Pyrenees
- Pomeranian
- Cairn Terrier
- American Cocker Spaniel
- Nova Scotia Duck Tolling Retriever
Prognosis Is Excellent, but the Medication Isn’t Cheap
Dogs with Addison’s disease live long and normal lives, but they do require the necessary medications.
One problem with management of the disease is cost.
The mineralocorticoid replacement can be a financial hardship, particularly in those larger breeds mentioned above. Both the injection (Percorten) and oral tablets (Florinef) are pricey.
Veterinarians try to keep these dogs happy and healthy but also must work with clients who are having trouble affording the medication.
Some people with large-breed dogs have considered euthanasia because they cannot fathom 7–8 years of expensive medication.
For these clients, the best we can do is to try and get the dog on the least amount of medication possible to control symptoms and keep the dog in a balanced state. Of course, the last thing we want is to give too little medication and send the dog into a crisis, adding veterinary expense.
As long as dogs with Addison’s disease get their medication and are monitored in times of stress, they can lead happy, normal lives.
Hopefully in the future, the medications will come down in price.
For more on Addison’s disease in dogs, watch this video from Dr. Karen Becker, DVM:

References
- Klein, Susan C., DVM, and Mark E. Peterson, DVM, DACVIM. “Canine Hypoadrenocorticism: Part I.” Canadian Veterinary Journal 51, no. 1 (January 2010): 63–69. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2797351/.
- Lathan, Patty, DVM, DACVIM, and Ann L. Thompson. “Management of Hypoadrenocorticism (Addison’s Disease) in Dogs.” Veterinary Medicine 9 (February 2018): 1–10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6055912/.
- “Vetoryl Capsules (Trilostane).” Dechra Veterinary Products. 2015. https://www.dechra-us.com/Admin/Public/Download.aspx?file=Files%2FFiles%2FSupportMaterialDownloads%2Fus%2F01TB-VET50030-0615.pdf.
- Webb, Craig, DVM, PhD, DACVIM, and David Twedt, DVM, DACVIM. “Acute Hepatopathy Associated With Mitotane Administration in a Dog.” Journal of the American Animal Hospital Association 42, no. 4 (July–August 2006): 298–301. https://pubmed.ncbi.nlm.nih.gov/16822769/.
- Macintire, Douglass, DVM, DACVIM, DACVECC. “Addisonian Crisis (Proceedings).” dvm360. Aug. 1, 2008. http://veterinarycalendar.dvm360.com/addisonian-crisis-proceedings.
- Hoskins, Johnny D., DVM, PhD, DACVIM. “Testing for Addison’s Disease.” dvm360. Jan. 1, 2009. http://veterinarynews.dvm360.com/testing-addisons-disease?id=&sk=&date=&pageID=2.
- Edwards, Scott H., BVMS, PhD. “Corticosteroids.” Merck Veterinary Manual. https://www.merckvetmanual.com/pharmacology/anti-inflammatory-agents/corticosteroids.
- Schaer, Michael, DVM, DACVIM, ACVECC. Clinical Medicine in the Dog and Cat. Manson Publishing Ltd. 2002.
 This pet health content was written by a veterinarian, Dr. Debora Lichtenberg, VMD. It was last reviewed June 25, 2019.
This pet health content was written by a veterinarian, Dr. Debora Lichtenberg, VMD. It was last reviewed June 25, 2019. 

