
Occasionally, I come across a client who point-blank refuses to give their dog an anesthetic. Sadly, this is usually because they once lost a much-loved pet under anesthesia.
Chatting further, it often transpires the tragedy happened years ago. Back then, anesthetic agents and protocols weren’t as sophisticated as they are today.
Discussing how gentle modern anesthetic agents are often puts minds at rest enough to go ahead with the procedure.
However, another reason for refusing is “The breeder says this breed dies under anesthetic.” While the delivery of the message is a little blunt (and oversimplified), sometimes there is a modicum of truth in what the breeder said.
Breed-Related Myths
We’ve heard it all:
- “Chihuahuas are more sensitive to anesthesia…”
- “Cocker Spaniels are more sensitive to anesthesia…”
- “Greyhounds are more sensitive to anesthesia…”
However, the reality is quite different when you look at scientific facts. Breed sensitivities to anesthesia in dogs are pretty much a myth, despite whatever your breeder, your best friend or your groomer may claim.
There is one drug that Greyhounds are very sensitive to: barbiturates. However, these drugs are no longer available in the United States, so they’re not really a concern anymore.
To be fair, some breeds and certainly some individuals can respond to some drugs differently. For example, Northern dog breeds such as Huskies tend to vocalize after receiving injectable pain medications related to morphine. Then again, if you have a Husky, you probably know they are quite vocal to begin with.
With all this in mind, let’s look at some of the breed-specific conditions that affect an anesthesia and what your vet does to keep the dog safe.
Flat-Faced Breeds: Pug, Bulldog and Boston Terrier
A vet’s heart is liable to start racing when they see a squish-faced breed on the operating schedule.
Bulldogs and other brachycephalic (flat-faced dogs and cats) breeds have a significantly higher risk for respiratory complications around anesthesia time.
When awake, these dogs often struggle to breathe, and anesthesia is an extra challenge, but your vet knows this and therefore anticipates the risks.
What many Bulldog folks don’t understand is that their anesthesia is very safe. The most critical period is after surgery. Bulldogs sometimes need an extended recovery period. The technician should monitor them closely until they are fully awake before removing the tube from their wind pipe.
Some of the challenges facing a flat-faced breed include:
- Large tonsils and a long soft palate blocking the back of the throat.
- A windpipe that is much narrower than it should be.
- A tendency to inhale saliva into the lungs.
To keep your dog safe, the vet will be proactive and will:
- Place an intravenous catheter for direct access to the bloodstream.
- Give the dog oxygen ahead of handling.
- Use low doses of sedatives so the dog has better control of their swallowing.
- Give anesthetic agents that wear off rapidly so the dog wakes quickly.
- Place a tube in the dog’s windpipe to maintain an open airway.
- Monitor the dog constantly until fully awake.
Sighthounds: Greyhound, Whippet and Saluki
These guys have an unusually low amount of body fat, which alters how they handle anesthetic agents.
Once upon a time, the anesthetics available meant these dogs slept for days afterward. Happily, this is no longer the case.
Modern drugs are short-acting and don’t rely on body fat soaking them up for the dog to wake up.
Was YOUR Pet Food Recalled?
Check Now: Blue Buffalo • Science Diet • Purina • Wellness • 4health • Canine Carry Outs • Friskies • Taste of the Wild • See 200+ more brands…

From the inductions agents to the gas that keeps the dog asleep, anesthetic protocols for sighthounds are almost unrecognizable from 10–20 years ago.
This means the dogs are fully awake within hours, just like any other dog.
However, sighthounds do seem to have too much of a blood clot-busting enzyme that leads to excessive bleeding. This is a risk you should discuss with your vet before any surgical procedure. For more on this, see our article “How Minor Surgery Could Put Your Greyhound in Danger.”

Herding Dogs: Border Collie and Australian Shepherd
Dogs of herding heritage are special cases.
A quirk in their physiology makes them overly sensitive to certain drugs, such as Ivermectin. This also applies to certain sedatives, but your vet knows this and uses low doses to compensate.
Toy Breeds: Chihuahua and Pomeranian
The teeny-tiny toy breeds have a large surface area relative to their size.
The upshot of this is they lose heat easily, especially under anesthetic. Heat pads and a particularly comfy sort of doggy hot air bed (called a “bear hugger”) ensure this isn’t a problem.
Another potential concern is a toy dog’s tendency toward low blood sugar. Careful monitoring during the anesthetic helps the vet tech and vet keep abreast of sugar levels so they know if an intravenous supplement becomes necessary.
Giant Breeds: Newfoundland and St. Bernard
These boys may be big, but they’re small at heart.
Many giant breeds are especially sensitive to sedative drugs, but your vet anticipates this by giving reduced dosages.
Special Mentions: Boxer, Doberman and Dachshund
Some breeds have issues all of their own, such as the Boxer’s extreme sensitivity to sedatives, the Doberman’s risk of silent heart disease or clotting problems, and the Dachshund’s inclination to a low heart rate under anesthetic.
Forewarned is forearmed, so your vet may wish to run tests ahead of the procedure to troubleshoot for problems.
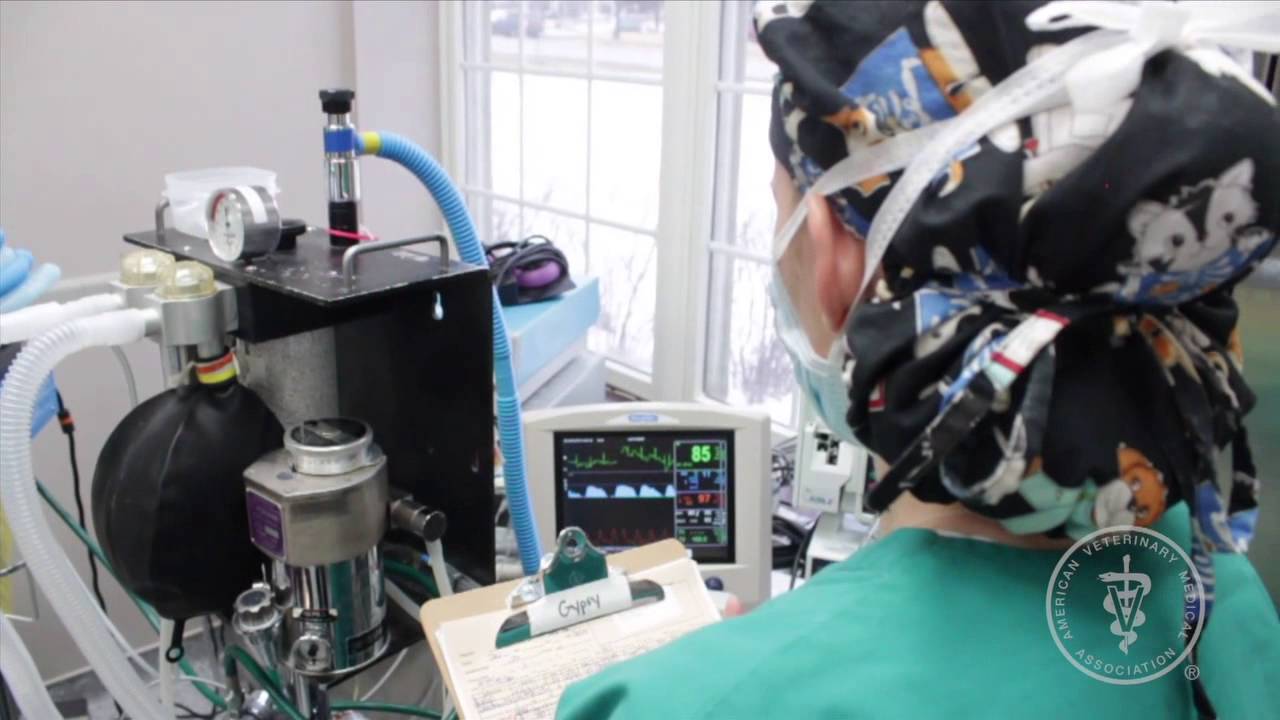
Learn more about what happens when your pet goes under from this veterinary anesthesiologist:
“But My Dog Is Too Small for Anesthesia!”
Not true.
All drugs, including anesthesia drugs, are calculated based on the pet’s weight, so whether your dog weighs 2 pounds or 102 pounds, they will get each drug based on their exact body weight the day of anesthesia.
Small patients have a higher risk of hypothermia (low body temperature), so they will be kept warm before, during and after anesthesia.
“But My Dog Is Too Old for Anesthesia!”
Again not true. “Age is not a disease,” as the saying goes.
Don’t use advanced age as an excuse to avoid a surgical or dental procedure under anesthesia that may benefit your pet’s health.
As long as pre-anesthetic blood work, physical exam, and possibly X-rays or an ultrasound are performed to be sure that vital organs are functioning well, older pets can safely go under anesthesia.
Geriatric patients may need an anesthesia protocol that is tailored to their needs, and your vet was trained to make such adjustments. In complicated situations, a board-certified anesthesiologist can be consulted.
“My Dog Can’t Go Under Anesthesia Because of a Heart Murmur”
Patients with heart conditions do need special attention.
Pre-anesthetic radiographs of the lungs and heart and an ultrasound of the heart should be done to assess the severity of the heart condition and determine if treatment is needed.
Anesthetic complications, no matter how rare, do happen.
It is our job to minimize them by hiring well-trained nurses, performing pre-anesthetic physicals, using modern monitoring equipment and tailoring anesthesia protocols to each patient.

Rather Than Refuse, Ask Questions Instead
You can’t bear the thought of putting your dog under anesthesia — and I totally get it.
There’s a risk with any anesthetic that no one can deny. But what many people don’t appreciate (probably because vets don’t tell them) is that each pet is treated as an individual.
There’s no “one size fits all” when it comes to anesthetic.
Each patient’s risk factors are carefully assessed and addressed, and everything is tailored to the individual, including screening blood tests, intravenous fluids, drugs, dosages and anesthetic circuits. Taking the pre-med injection as an example, there’s a whole array of different drugs available to best match a patient’s age, breed or health conditions.
In short, discuss your concerns with the vet. Chances are they’re way ahead of you in terms of risk assessment.
No one will force you to do anything you don’t want to, but perhaps when you know all the facts, you may feel a little better about trusting professionals with your dog’s care and a little less like taking the breeder’s word as gospel.
This pet health content was written by a veterinarian, Dr. Pippa Elliott, BVMS, MRCVS, with contributions from Dr. Phil Zeltzman, DVM, DACVS, CVJ, and Kelly Serfas, a certified veterinary technician. This article was reviewed for accuracy by Dr. Elliott and was last updated Dec. 17, 2018.



